
Content Reviewed by:
Dov Apfel
Content Reviewed by: Dov Apfel
Accordion Content
Since 1979, Dov Apfel has been passionate about advocating for birth injury and medical malpractice victims. Mr. Apfel’s career-long record of achievements in birth injury litigation, education, and advocacy has been recognized by the Executive Board of the Birth Trauma Litigation Group of the American Association for Justice. His expertise is demonstrated by his numerous awards, presentations on birth injury topics at legal conferences for organizations like the AAJ and ATLA, and articles published by Trial Magazine and many others.
Hypoxic-ischemic encephalopathy, or HIE, is a type of birth asphyxia that occurs when a baby is deprived of oxygen before, during, or after birth. This results in brain cells lacking the energy they need to function. In moderate and severe HIE, this is followed by a short recovery period and a secondary loss of cellular energy, during which more significant damage may occur.
The Sarnat staging criteria were originally developed in 1976 during a study of 21 newborn infants with HIE and used in conjunction with an electroencephalogram, or EEG, to assess symptoms’ severity and each case’s likely outcome. This system is still widely used today. Families facing the challenges of HIE may find it beneficial to seek support from medical professionals and, when appropriate, explore legal options with a birth injury lawyer.
Diagnosing Hypoxic-Ischemic Encephalopathy
The Apgar scale is a scoring system used in delivery rooms to quickly assess a newborn’s health after the birthing process. It is generally performed one minute and five minutes after birth, with the highest possible score being 10. A normal Apgar score is seven or higher.
A healthy newborn infant should be alert with good muscle tone and multiple reflexes, which include the following, according to the Icahn School of Medicine at Mt. Sinai:
- Moro reflex – flailing of the arms to the sides with palms up and a startled look in response to a falling sensation
- Sucking reflex – making sucking motions when the mouth is touched
- Grasping reflex – grasping a finger placed in the open palm
- Tonic Neck Reflex – when moved to one side, one hand is a tight fist while the other is relaxed and open, with these changing if the baby’s position is changed
Hypoxic-ischemic encephalopathy may be diagnosed when the following symptoms are observed:
- Low umbilical artery blood pH, indicating acidemia
- Apgar score of 3 or less for longer than five minutes
- Seizures
- Coma
- Low muscle tone
- Damage or failure of multiple organs
- Weak, absent, or overly strong reflexes
After the initial diagnosis of HIE, further testing and evaluation is performed to determine the stage. It is important to perform this assessment as quickly as possible to ensure treatment commences early enough for a therapeutic benefit.
What Are the Stages of Hypoxic-Ischemic Encephalopathy?
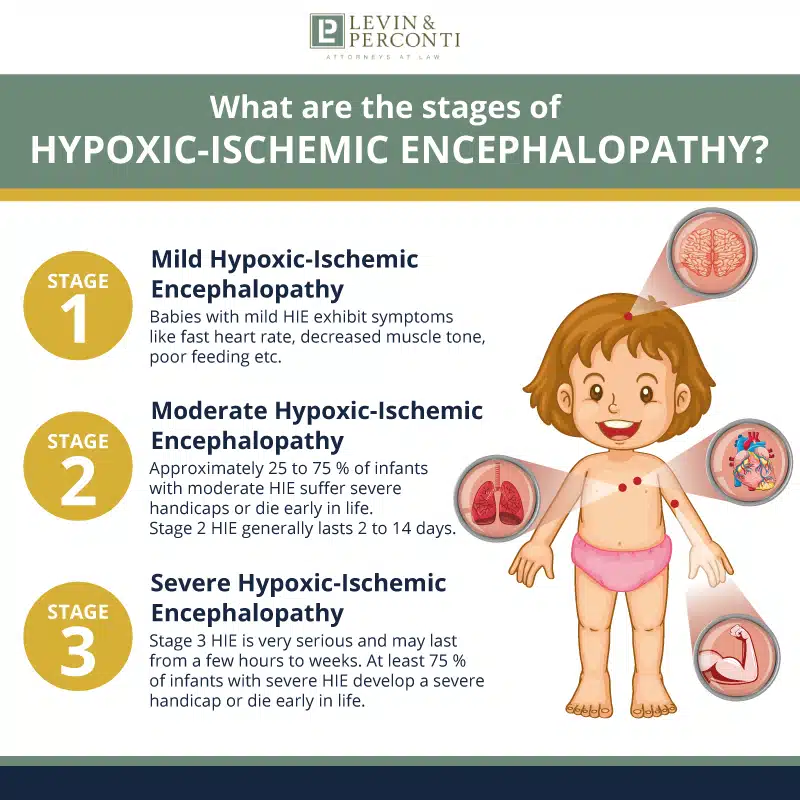
Hypoxic-ischemic encephalopathy occurs in the following three stages:
- Stage 1: Mild hypoxic-ischemic encephalopathy
- Stage 2: Moderate hypoxic-ischemic encephalopathy
- Stage 3: Severe hypoxic-ischemic encephalopathy
Stage 1: Mild Hypoxic-Ischemic Encephalopathy
Babies with mild HIE may exhibit the following symptoms:
- Hyper-alertness
- Fast heart rate, or tachycardia
- Slightly decreased muscle tone
- Stronger deep tendon reflexes
- Poor feeding
- Excessive crying
- Irritability
- Sleepiness
EEG results are typically normal during stage 1 HIE, and the infant is generally awake. This phase may last for one to three days. Stage 1 HIE can worsen and progress to Stage 2, but it typically resolves within 24 hours without further progression.
A study by JAMA Pediatrics found that two-year-old children with mild HIE scored lower than their peers without HIE during cognitive testing, and they did not score higher than children who had moderate HIE who received therapy.
Stage 2: Moderate Hypoxic-Ischemic Encephalopathy
Approximately 25 to 75 percent of infants with moderate HIE suffer severe handicaps or die early in life. Stage 2 HIE generally lasts 2 to 14 days. Symptoms include the following:
- Lethargy
- Significantly deficient muscle tone
- Lack of deep tendon reflexes
- Deficient or absent Moro, sucking, and grasping reflexes
- Breathing problems
- Seizures within 24 hours after birth
- A sudden deterioration after an initial period of well-being
- Flexed arms
- Extended legs
- Hyperactive or decreased stretch reflexes
- Small pupils
- Slow heartbeat
- Diarrhea
Seizure activity may increase after a sudden deterioration following a period of well-being. Stage 2 HIE may be present at diagnosis or have progressed from stage 1. Stage 2 can progress to stage 3, but this does not always occur.
Stage 3: Severe Hypoxic-Ischemic Encephalopathy
Stage 3 HIE is very serious and may last from a few hours to weeks. At least 75 percent of infants with severe HIE develop a severe handicap or die early in life. Symptoms may include the following:
- Stupor
- Coma
- Unresponsiveness
- Irregular breathing, often requiring ventilation
- Lack of deep tendon reflexes
- Deficient muscle tone throughout the body
- Absent neonatal reflexes
- Irregular eye movements
- Unresponsive or dilated pupils
- Seizures 24-48 hours after the initial injury
- Deterioration of consciousness, suggestive of cerebral edema
- Irregular heartbeat
- Hypertension
- Death from cardiorespiratory failure
How Does Hypoxic-Ischemic Encephalopathy Progress?
Stage 1 hypoxic-ischemic encephalopathy generally resolves without secondary injuries, but infants with stages 2 and 3 HIE generally experience a predictable chain reaction of events that stem from the initial deprivation of oxygen and loss of blood flow to the brain.
Primary Energy Failure
The purpose of blood flow is to deliver nutrients to all body parts. Oxygen and glucose are two of the most important nutrients that provide the brain with energy. The brain is deprived of both substances during primary energy failure, also known as the acute phase of hypoxic-ischemic encephalopathy.
As a result, the brain becomes deficient in adenosine triphosphate (ATP), which essentially powers the brain.
This triggers lactic acid production as the body attempts to provide the brain with an alternative energy source. Lactic acid causes blood vessels to dilate, leading to brain swelling. Lactic acid also leads to a failure of the body’s sodium potassium pump, resulting in excess calcium entering the cells.
Excess intracellular calcium causes a series of chemical reactions in the brain that ultimately lead to excess fluid in the brain, DNA fragmentation, restricted blood flow to the brain, and cell death.
In moderate and severe HIE, the buildup of reactive oxygen species in the tissues, also known as free radicals, damages the brain and other vital organs. Multiorgan dysfunction is common in moderate and severe hypoxic-ischemic encephalopathy cases, most commonly impacting a combination of the following organs:
- Heart
- Lungs
- Kidneys
- Liver
- Blood
One of the primary drivers of multiorgan failure in HIE is low blood pressure, which affects approximately 62 percent of HIE patients, according to Frontiers in Pediatrics.
Cell Death
Two types of cell death occur during primary energy failure: necrosis and apoptosis.
Necrosis occurs when cells swell and rupture. This results in the destruction of the cellular membrane and a subsequent release of the cellular contents into the surrounding area. This increases inflammation. Necrosis is most prevalent in Stage 3 HIE.
Apoptosis occurs when cells shrink and die without damaging the cellular membrane or causing inflammation. While apoptosis is a less damaging process, both apoptosis and necrosis can lead to impaired brain function.
The Latent Period
The latent phase of HIE is a period of recovery that occurs in stage 2 and 3 HIE patients. It is characterized by a restoration of blood flow to the brain. It may last one to six hours. If the infant is a candidate for therapeutic interventions, the optimal timing is generally during this stage.
During this period, blood, oxygen, and nutrients are reintroduced into the brain tissues, and the brain returns to normal oxygen consumption. However, the damage done during primary energy failure is still present, and neuroinflammation and cell death reactions continue. Inevitably, the latent period gives way to secondary energy failure.
Secondary Energy Failure
Secondary energy failure occurs approximately six to 48 hours after the acute stage in stage 2 and 3 HIE cases. The damaging effects are often more severe than during primary energy failure. However, the initial injury’s severity influences this phase’s severity.
During secondary energy failure, the brain experiences an additional injury known as reperfusion or hyperperfusion, which involves an excessive blood flow to the brain. The exact mechanisms responsible for this stage are still under investigation, but researchers believe the following mechanisms are responsible:
- Angiogenesis – the formation of new blood vessels immediately following the initial injury
- Cerebral vasodilation – an increase in the diameter of the blood vessels in the brain
- Oxidative stress – the presence of too many unstable molecules known as free radicals as a result of oxygen deprivation
- Excitotoxicity – overstimulation caused by an excess of the neurotransmitter glutamate
- Inflammation – leads to edema due to the influx of white blood cells in the brain tissues
Oxidative stress is typically managed by antioxidants, which fight off free radicals, but newborn infants have a low level of antioxidants in the brain. At the same time, they consume more oxygen as a result of the transition to life outside the womb.
Excitotoxicity may lead to excess sodium and calcium in the cells, leading to long-term impairments of the following:
- Hearing
- Vision
- Somatosensory function
- Learning
- Memory
- Child development
The damage caused by this stage ultimately leads to increased cell death and sets the stage for injury to other bodily organs.
The Tertiary Phase of Moderate and Severe HIE
The tertiary phase occurs during the weeks and months following secondary energy failure. The baby’s alertness may improve approximately four to five days following the initial injury, and the brain attempts to repair and remodel itself. The brain may continue to experience damage for months to years.
Normal brain development during the early years of a child’s life is characterized by a rapid increase in neurons and synapses as the child learns and adapts to the world. Neural plasticity is the brain’s ability to form new pathways to facilitate adaptation. It is most pronounced during infancy and early childhood.
The brain damage caused by moderate and severe HIE can inhibit the development of new neurons and reduce plasticity. This can cause ongoing brain damage and impaired development.
Children with moderate to severe HIE may continue to have reduced muscle tone and associated difficulties with feeding, resulting in a need for tube feeding for weeks or months.
Can a Baby Fully Recover from HIE?
A baby can recover from HIE without long-term effects, but it is more common in mild cases. According to News-Medical Life Sciences, 10 to 60 percent of infants with HIE do not survive, and of those that do, approximately 80 percent have long-term neurological deficits.
Treatment for HIE
Therapeutic hypothermia, or cooling therapy, is the sole therapeutic treatment available for patients with HIE. Cooling therapy for HIE involves gradually cooling an infant’s whole body or brain to approximately 92° Fahrenheit for 72 hours, after which the infant is gradually rewarmed.
This treatment is generally considered safe with mild side effects, but it requires continuous monitoring of the baby’s vital signs during the cooling and rewarming stages. Complications that may occur without careful monitoring include the following:
- Bedsores
- Too much fluid in the tissues, or hypovolemia
- Kidney impairment following treatment
- An increased risk of developing necrotizing enterocolitis
- Infant distress from cooling, which could negate therapeutic effects
- Blood clots
- Slowed metabolism of drugs, resulting in higher blood concentrations
- An increased risk of seizures during the rewarming phase
For it to be effective, cooling therapy must begin within six hours after the onset of HIE, during the latency period between primary and secondary exposure. The goal is to prevent secondary energy loss. This underscores the importance of a timely diagnosis by medical personnel.
Unfortunately, cooling therapy only benefits one in eight infants that receive it for moderate or severe HIE. Additionally, not all babies with hypoxic-ischemic encephalopathy are candidates for therapy.
Infants who cannot receive cooling therapy will receive care aimed at supporting the affected organs, including the following:
- Monitoring of the heart
- Blood pressure monitoring and control
- Kidney and liver function support
- Mechanical ventilation
- Oxygen supplementation
- Medical control of seizures
Possible long-term effects of HIE
Hypoxic ischemic encephalopathy is associated with a high mortality rate, even after the infant leaves the neonatal intensive care unit (NICU). According to two studies published by Medscape, 37 to 38 percent of HIE patients who survived the NICU had died before their 18 to 22-month follow-ups. In addition, the following neurodevelopmental outcomes were observed at 18 months:
- Impaired mental development
- Impaired motor development
- Disabling cerebral palsy
- Epilepsy
- Blindness
- Severe hearing impairment
These conditions may persist throughout life.
Levin & Perconti Can Help
Medical malpractice may be to blame if your baby suffered HIE during birth and has experienced subsequent long-term effects. Hypoxic-ischemic encephalopathy is often preventable and may occur as a result of the following errors:
- Failure to perform a timely caesarian
- Failure to diagnose HIE
- Delayed diagnosis of HIE
- Failure to timely commence cooling treatment
Our hypoxic-ischemic encephalopathy lawyers at Levin & Perconti have more than 200 years of combined experience helping victims of medical malpractice recover substantial compensation and get justice for the negligence leading to their injuries.
We have recovered millions on behalf of children who experienced hypoxic-ischemic encephalopathy, including the following:
- $40 million verdict on behalf of the now 19-year-old woman who suffered a severe and permanent brain injury during birth due to a delayed C-Section delivery
- $20 million verdict for a child who suffered preventable HIE at birth, resulting in permanent cognitive and developmental impairments
- $11.5 million settlement for a child born at the U.S. Naval Hospital in Guam who suffered a catastrophic hypoxic-ischemic brain injury from negligent neonatal resuscitation and intubation
- $3.5 million settlement for the family of a baby who suffered a hypoxic-ischemic brain injury resulting in multiple medical complications that ultimately led to the child’s death
Hypoxic-ischemic encephalopathy is often preventable. If your child developed this condition and passed away or experienced subsequent complications, we can help you identify the responsible parties and the errors that caused the condition. This will enable our birth injury attorneys to file a medical malpractice lawsuit on your child’s behalf.
Our compassionate attorneys have seen firsthand the devastation parents experience because of HIE, and we understand the tremendous financial and emotional strain this can cause your family.
While financial compensation cannot undo the harm, it can ensure you have access to the care and support your child needs for as long as your child needs it. Contact us today for a free consultation.



