Nursing Home Abuse & Neglect
Nursing home abuse is a horrifying reality happening in our communities and affecting our senior citizens. When we place our elder loved ones in a nursing home, we expect staff members to treat them with dignity and respect. Unfortunately, that’s not always the case.
With over 15,000 nursing homes housing 1.7 million licensed beds across the United States as of 2016 and current residents totaling upwards of 1.3 million as of 2015, nursing homes and staff need to be held accountable for how they care for our older generations. Therefore, it’s crucial to understand what nursing home abuse is, the different types of abuse, signs of abuse, and how to prevent it.
What is Nursing Home Abuse?
The Administration on Aging, an agency of the U.S. Department of Health and Human Services, defines elder abuse as “any knowing, intentional, or negligent act by a caregiver or any other person that causes harm or a serious risk of harm to a vulnerable adult.”
A long-term study showed that elder abuse victims are twice as likely to die prematurely than individuals who have not suffered from elder abuse. Nursing home abuse, which refers to elder abuse in a nursing home, can lead to serious physical injuries, emotional harm, and even death.

Types of Nursing Home Abuse
There are different types of elder abuse in nursing homes, including physical abuse, emotional abuse, sexual abuse, neglect, and exploitation.
1. Physical Abuse
Physical neglect includes anything that deprives residents of their primary needs for survival and dignity, including food, warmth, shelter, and a sanitary environment. Physical abuse in nursing homes happens whenever a resident suffers bodily harm, pain, or impairment because of mistreatment or neglect. Physical abuse can consist of:
- Active abuse (hitting, punching, slapping, kicking, etc.)
- Physical neglect
- The misuse of physical restraints
In nursing homes, staff members are only supposed to use restraints for medical reasons and for a short time. Keeping restraints on patients for long periods can reduce muscle tone and bone mass and cause muscle disorders and other serious injuries.
Nursing home caregivers, visiting family members, and other residents are the primary abusers in nursing homes. Studies show that physical abuse is often committed as a form of retaliation by nursing home staff against physically aggressive patients acting out often due to dementia and other conditions resulting in mental decline.
2. Emotional Abuse
Emotional abuse generally refers to any non-physical, verbal abuse, including:
- Insults
- Harassment
- Yelling
- Threats
Emotional abuse can also include depriving a patient of their dignity, for example, by leaving them in soiled clothes or refusing to allow them to make choices over daily decisions. According to a World Health Organization study from 2020, emotional abuse is the most common type of elder abuse. Almost a third of all nursing home employees have admitted to emotionally abusing a patient.
3. Neglect
Neglect refers to a caretaker’s failure to provide food, shelter, medical care, or protection. General and medical neglect can lead to:
Neglect is different from abuse in that it usually refers to an unintentional act. An example of neglect is if a nursing home resident wanders from the premises and dies from hypothermia while lost outside. Another example is when a nursing home employee fails to change a resident’s position in bed and, as a result, the resident develops bedsores.
4. Sexual Abuse
Sexual abuse is any non-consensual sexual contact. Unfortunately, this type of abuse is a prevalent form of elder abuse. Common signs of sexual abuse include bruises around the breasts or genital areas and unexplained sexually transmitted diseases.
5. Financial Exploitation
Financial exploitation refers to the illegal taking, misuse, or concealment of funds or property. Older people, particularly those with dementia or cognitive decline, are particularly susceptible to financial fraud, and criminals know this.
In July 2021, a nursing home employee in Pennsylvania was convicted of stealing more than $500,000 from residents of a nursing home. The man stole checks from the residents and then forged their signatures and cashed them at various banks.
Signs that Someone May Be Abusing Your Elderly Loved One
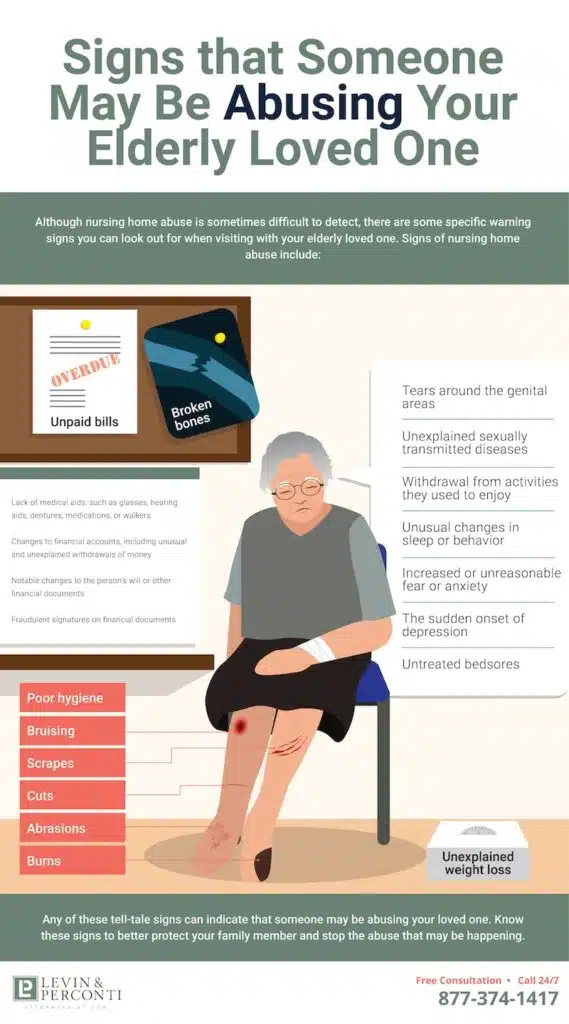
Although nursing home abuse is sometimes difficult to detect, there are some specific warning signs you can look out for when visiting with your elderly loved one. Signs of nursing home abuse include:
- Bruising
- Broken bones
- Scrapes
- Cuts
- Abrasions
- Burns
- Tears around the genital areas
- Unexplained sexually transmitted diseases
- Changes to financial accounts, including unusual and unexplained withdrawals of money
- Notable changes to the person’s will or other financial documents
- Fraudulent signatures on financial documents
- Unpaid bills
- Withdrawal from activities they used to enjoy
- Unusual changes in sleep or behavior
- Increased or unreasonable fear or anxiety
- The sudden onset of depression
- Untreated bedsores
- Poor hygiene
- Unexplained weight loss
- Lack of medical aids, such as glasses, hearing aids, dentures, medications, or walkers
Any of these tell-tale signs can indicate that someone may be abusing your loved one. Know these signs to better protect your family member and stop the abuse that may be happening.
Frequent Slips and Falls
Because slips and falls by older people can quickly lead to death, nursing home employees must monitor vulnerable residents at risk of falling. Specifically, individuals with cognitive problems or physical impairments are at high risk.
You may notice that your loved one has recently had frequent slips and falls. Falling often may be a sign of elder abuse or neglect.
Malnutrition/Dehydration
Our bodies need water to survive. Water gets rid of bodily wastes through urination, sweating, and bowel movements. These processes keep the body’s temperature regular, lubricate joints, and protect tissues. Dehydration happens when the body is not functioning correctly because of too little water in the body.
Women need about 2.7 liters of water each day, and men need about 3.7 liters. Physical symptoms of dehydration include:
- A sticky and dry mouth
- Being thirsty
- Dry or papery skin
- Infrequent urination
- Dark yellow urine
- Confusion and irritability
- Delirium
- Breathing fast
- Low blood pressure
- Inability to sweat
Dehydration is a common problem among the elderly in many nursing homes, and it’s a sign of serious neglect. Nursing homes must ensure that residents get plenty of water. When an older person becomes dehydrated, they may lack a strong thirst drive and might not show any outward symptoms of lacking hydration. Chronic dehydration in elderly persons can lead to seizures, brain swelling, kidney failure, and even comas.
Malnutrition, or having insufficient nutrients in the body, is also a common sign of neglect in nursing home residents, with about 85% of nursing home residents suffering from this dangerous condition. Malnutrition can lead to weight loss, fatigue, weakness, yellowing skin, white fingernails, and bedsores.
The combination of dehydration and malnutrition in elderly persons can be particularly deadly. In one tragic case, a nursing home entered into a settlement of almost $1 million after a 91-year-old resident suffered from dehydration and malnutrition over three years. As a result, she lost a third of her body weight and ultimately died. Illinois nursing regulators subsequently shut down the nursing home due to her injuries and death and other reported abuse and neglect incidents.
Fractures
Fractures and bruises are common signs of physical abuse in nursing homes. If a nursing home is taking proper care of your loved one, they shouldn’t suffer from either of these conditions.
Falls often cause fractures and are particularly dangerous to an older adult. A fall may break the person’s hip, which can quickly lead to death. The nursing staff should be taking all necessary precautions to prevent elderly residents from falls.
Precautions should include ensuring that the residents use walkers, canes, or wheelchairs and have assistance when getting in and out of beds.
Bruises
Bruises can result from falls, bumps, and more severe injuries. Older people tend to bruise more easily than young people because their skin tissue is thinner and more delicate. In addition, the use of blood thinners by some elderly people may also increase the chances of bruising. Although bruises can occur in older adults without any accompanying neglect, they could also be a sign of abuse, so it’s important to pay extra attention to bruises apparent on your elderly loved one, mainly if they’re reoccurring or if they appear on the wrists or ankles, which might indicate misuse of restraints.
In 2017, a jury in Chicago awarded $2.7 million to the estate of a 67-year-old man who died from complications after he fell at a nursing home. The lawsuit alleged that a nurse at the nursing home should have given the man assistance when walking. He was known to suffer from cognitive impairment, decreased safety awareness, and a history of fainting. He fell in the entranceway of his room, suffering a skull fracture and two brain hemorrhages, and died about four months later.Incorrect Medication
If your elderly loved one received incorrect medication or lacks needed medication, this could be a sign of elder abuse. At the very least, it shows that the nursing home didn’t properly train their nursing staff. Errors in administering medication include:
- Crushing medication that shouldn’t be crushed
- Not providing food or water with the medication
- Giving the medication at the wrong time or giving an incorrect dosage
- Giving the patient expired medication
- Overmedicating residents in nursing homes to subdue or control them
One common form of nursing home abuse is giving residents medications they don’t need for the sole purpose of sedating them when it’s not medically necessary. Signs that your loved one has received incorrect medication include changes in their behavior, unexplained weight loss or weight gain, confusion, memory loss, and lethargy.
In one tragic case involving medication mismanagement, a jury in Chicago returned a $4.1 million verdict for an 85-year-old woman who suffered from a stroke after nursing home staff inexplicably stopped giving her an anti-stroke drug, despite no doctor having ordered discontinuation of the medication. Not only did the nursing staff stop giving the plaintiff her much-needed medicine, but they also failed to detect their error in their required daily audits. The woman lived for four more years after the stroke, but her quality of life declined significantly following the incident.
Bedsores
Bedsores develop when a person spends long periods in a chair or bed without moving around. Signs of bedsores are discolored or painful skin and open wounds on parts of the body, usually the hips, buttocks, back, and ankles. Bedsores are a sign of neglect because nursing home employees must move elderly patients who can’t move around by themselves. Bedsores can lead to serious medical complications and even death.
In one recent lawsuit, an assisted living facility and the surviving family of an 88-year-old assisted living resident reached a $2.3 million settlement. The assisted living facility failed to take care of the resident, causing them to develop severe and infected bedsores, leading to their eventual death.
Withdrawn Behavior
If you’ve noticed your loved one withdrawing from activities they used to enjoy, or if they seem suddenly depressed, they may be suffering from elder abuse. Withdrawn behavior can be a sign of numerous types of abuse, including physical, emotional, and sexual abuse. Of course, withdrawn behavior is not always an indicator of abuse, as it might also be a sign of increasing cognitive decline. Still, it can sometimes be a red flag, so it’s not something you should ignore or readily dismiss.
Anything That Doesn't Seem Right
Finally, you may notice that something just doesn’t seem right with your loved one. Always trust your instincts if something seems “off.” If something seems strange, such as a pair of broken glasses, changes in behavior, changes in finances, or other things that pique your curiosity, certainly don’t disregard your concerns without further investigation.
Why Does Nursing Home Abuse Happen?
There’s no single cause for nursing home abuse. However, several factors usually work together to create abusive and dangerous environments for older adults in nursing homes. Usually, an abusive nursing home situation shares a link to the nursing home’s owner or administrator, which has decided to place profits over ensuring the safety of the residents. As of 2016, almost 70 percent of all nursing homes were for-profit businesses, sometimes creating cause for concern about one’s motives.
In some cases, owners of nursing homes may forego needed repairs or might neglect to adequately screen employees. Inadequate training, high staff turnover, and low staff to resident ratios can also lead to increased instances of elder abuse and neglect. For example, an improperly trained staff member may give a patient food they’re not supposed to eat, or they might not know how to perform CPR or check for bedsores, and they might even administer the wrong medications. Since senior citizens are at a higher risk of being abuse victims, nursing homes should implement heightened measures to ensure their safety.
In a heartbreaking example of the dangers of lack of training, a jury entered a $1 million verdict in a lawsuit against an assisted living facility. In this particular abuse case, the nursing home admitted that understaffing and insufficient training led to a 67-year-old man’s choking death after staff members failed to feed him a mechanical soft diet.
Additionally, inadequate staffing can lead to burnout, stress, and mistakes. Nursing home employees tend to work for low pay under stressful and unpleasant conditions, leading to employee depression or substance abuse. A stressed and underpaid employee may take out their frustrations on innocent patients in nursing homes. Of course, there is never any excuse for this behavior. Nursing home abuse violates state and federal laws, it’s often a crime, and it should never happen to your loved one or any other elderly individual.
Alzheimer's/Dementia Abuse
Nursing home residents with Alzheimer’s, the most common form of dementia, are especially vulnerable to abuse. A study published in the Journal of the American Geriatrics Society found that almost half of all patients with dementia suffer from abuse or neglect. In addition, patients with dementia are the most likely to suffer from financial abuse or exploitation.
The reason for dementia patients’ increased risk of abuse is because abusive caregivers know that persons with this form of cognitive decline have difficulty remembering, reasoning, and communicating, making them easy targets for financial fraud. For instance, a caregiver may convince the dementia patient to change their will to leave their money to the caregiver. Signs of financial abuse include missing cash or valuables, unexplained money withdrawals, and unpaid bills.

Nursing Home Abuse Statistics
According to the U.S. Department of Justice (DOJ), each year, about one of every ten people over 65 suffer from elder abuse in the United States. According to the National Institutes of Health (NIH) and the National Center on Elder Abuse, women are more likely than men to be victims of elder abuse.
Elder abuse occurs more often in nursing homes and long-term care facilities than in other places, such as elderly persons’ homes. A study published in 2018 in the European Journal of Public Health found that about 15 percent of older adults in institutional settings (as opposed to home-based care) suffer from elder abuse worldwide. However, this number is likely low, as elder abuse is often unreported.
A recent study by the World Health Organization (WHO) shows that, in institutional settings, the most common form of abuse is psychological abuse (about 33%), followed by physical abuse (about 14%), financial abuse (about 13%), neglect (about 11%), and sexual abuse (about 2%).
Nursing home abuse is a serious problem in the U.S., and evidence suggests that nursing home abuse is almost as common as child abuse. Half of all nursing home staff have admitted to mistreating their elderly patients through physical violence, mental abuse, or neglect. Studies indicate that while nursing home staff, medical personnel, other patients, family, and visitors commit some of the abuse, orderlies and aides commit most of the abuse in nursing homes.
Older adults living in nursing homes with long-term support systems are the most likely to become victims of elder abuse because these individuals often suffer from diseases or ailments that affect cognitive functioning and make them entirely dependent on other people.
Reporting Nursing Home Abuse
If you suspect your loved one is the victim of nursing home abuse, you should report the abuse immediately. First, report to the nursing home administrator. If the nursing home doesn’t address the problem, you should then contact the agency in your state that regulates nursing homes. Each state has an agency dedicated to preventing elder abuse, with procedures for reporting.
Under the federal Older Americans Act, first enacted in 1965, each state is required to establish an Ombudsman Program that serves to advocate for elderly persons, including residents of nursing homes and assisted-living facilities. Each state’s Ombudsman Program has procedures for reporting elder abuse. Contact the Ombudsman Program in the state where your loved one resides to report the abuse. You can also find reporting numbers through Eldercare Locator at 1-800-677-1116 or by going to eldercare.gov.
You can also contact your local sheriff’s office to report elder abuse, as it’s likely that the abuse constitutes a local or state crime.
Finally, set up a free consultation with an experienced nursing home abuse lawyer. We’re ready to help you recover from nursing home abuse and neglect and get the reimbursement you deserve.
How to Prevent Nursing Home Abuse
You can take several steps to help prevent nursing home abuse. First, know the signs. Next, check in regularly with your loved one. Third, raise any concerns with staff and authorities. Finally, be proactive in researching the nursing home and looking for any red flags. Federal regulations require nursing homes to report and investigate all allegations of abuse, neglect, misappropriation of resident property, and exploitation.
Nursing homes are also required to report any unexplained injuries. Again, search your state’s elder abuse agency for reports on a specific nursing home in the state. However, know that nursing home self-reporting doesn’t always accurately represent how the elderly care facility is being run. For example, the New York Times recently published a scathing article, accusing nursing homes of deliberately misrepresenting the quality of care provided and forging their figures to inflate their staff to resident ratios.
Therefore, it’s crucial to conduct your own investigation of the nursing home where your loved one is living. You should visit the home often and get to know your loved one’s primary caregivers personally. Ask lots of questions and actively look for signs of abuse.
Taking these measures could ultimately save your loved one’s life.
Legally Reviewed by

Steven M. Levin
Contact Us
- Free Consultation
- (312) 332-2872
"*" indicates required fields
Related Pages
- Alzheimer's Disease
- Bed Sores
- Broken Bones
- Chemical Restraints
- CILA Group Home Abuse
- Elder Abuse
- Falls
- Financial Exploitation
- Inadequate Training
- Malnutrition & Dehydration
- Medication Errors
- MRSA
- Overmedication
- Physical Restraints
- Poor Hygiene
- Sepsis
- Sexual Assault
- Understaffing
- Wandering & Elopement
- Wrongful Death
Notable Results
VERDICT
on behalf of an 85-year-old woman injured in a nursing home when her medications were mismanaged.
VERDICT
for the estate of a 67-year-old man who died from complications related to a fall
SETTLEMENT
for a 59-year-old resident who developed multiple painful and infected bedsores which took four years to heal.
FAQs
- What are the warning signs of nursing home abuse?
- What are the four stages of bedsores?
- How much is a bedsore lawsuit worth?
- How long does it take to get bedsores?
- Can you die from bedsores?
- What are the three stages of sepsis?
- How can nursing home falls be prevented?
- Are bedsores preventable?
- What Is nursing home liability insurance?
Our Office
325 N LaSalle Dr Suite 300
Chicago, IL 60654
312-332-2872